About CCI Support
We are an Aotearoa / New Zealand registered non-profit charity and our purpose is to improve the quality of life of people who live with complex chronic illnesses, as well as that of their loved ones.
With our support, people with complex chronic illnesses can, in time, develop an increased ability to participate in family, social, and community life, and lead a life that is fulfilling and meaningful for them.
Our vision to “Empower People Towards Wellness” is delivered through support services and resources offered to members by our Health & Wellness Facilitators and through our innovative award-winning “Towards Wellness” Programme. We work with our members, their families, and their community by providing practical tools and helping them to develop tangible next steps for their journey towards wellness.
CCI Support, is more than just an organisation; it’s a beacon of hope and understanding for those facing the challenges of chronic health conditions.
At CCI Support, we understand the unique struggles and uncertainties that come with managing chronic illnesses. That’s why we’re committed to providing comprehensive assistance and a supportive community for individuals and their loved ones every step of the way.
Illnesses We Support
Myalgic Encephalomyelitis (ME) / Chronic Fatigue Syndrome
Myalgic Encephalomyelitis, also known as Chronic Fatigue Syndrome (together referred to as ME/CFS), is a debilitating, long-term, multi-system illness. It can affect the immune, neurological, endocrine, and autonomic systems, leading to a wide range of confusing and disabling symptoms. It has been described as an abnormal immune system response to any number of infectious or environmental triggers, causing a long-term illness that can result in significant disability.
Known triggers are viral infection, or a myriad of triggers, including but not limited to adverse/allergic reactions to anaesthesia/vaccination, chemical toxicity, hormonal fluctuations (childbirth, menopause), physical/emotional trauma, and/or genetic predisposition. There is also emerging research to show genetic links.
Approximately 80% of cases are preceded by a viral infection, such as:
- Common cold
- Influenza
- Pneumonia
- Epstein-Barr virus/Glandular fever
- Herpes virus
- COVID-19
While many people recover from viral illness within a few weeks, those with ME/CFS do not return to full health and instead develop persistent, life-altering symptoms lasting at least six months prior to diagnosis for adults, and three months for children.
In the case of COVID-19, symptoms lasting beyond twelve weeks may be diagnosed as Long-COVID, and if they persist beyond two years, they may be considered Long-COVID–induced ME/CFS.
People who have compromised/weakened immunity or have pre-existing conditions may be more prone to ME/CFS. At present, there are few treatment options available for ME/CFS.
- Onset: Can be triggered by a viral infection, but it can also have a gradual onset without a clear viral trigger.
- Symptoms: Prolonged and severe fatigue, often accompanied by cognitive dysfunction (brain fog), unrefreshing sleep, and pain. The symptoms are not solely explained by ongoing viral activity or other medical conditions.
- Duration: ME/CFS is characterised by persistent symptoms that last for at least six months. The severity of symptoms can fluctuate, but the condition is chronic, lasting for years.
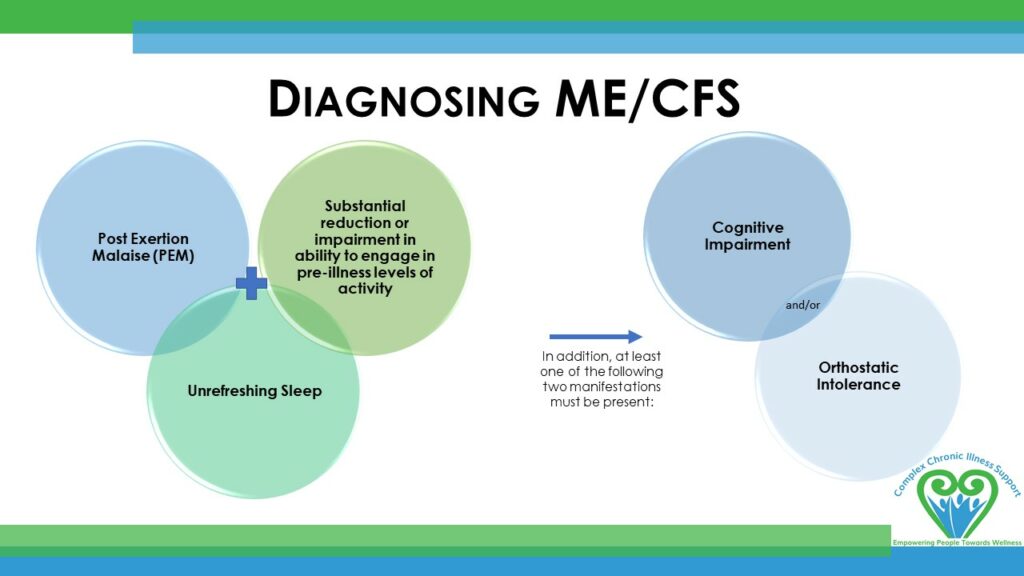
It's important to note that while post-viral fatigue can resolve on its own as the body recovers from the initial infection, ME/CFS is considered a chronic condition with a more persistent and often disabling course. The defining diagnostic characteristic of ME/CFS is post-exertional malaise (PEM) – a worsening of symptoms after even small amounts of physical, mental, or emotional effort, often delayed by 24–72 hours.
Main symptoms include:
- PEM
- Unrefreshing sleep
- Unrelenting fatigue that cannot be explained by other conditions
- and then 1 of: Orthostatic intolerance or cognitive impairment – impaired memory and concentration.
- Muscle and/or joint pains
- Sleep disturbance
- Digestive problems
- Sensitivities to light and sound
- Headaches/migraines
- Sore throat and/or enlarged lymph nodes
- Dysregulated temperature control – fever/chills
- POTS
- Orthostatic intolerance – erratic heart rate, feeling faint or dizzy upon standing
- Anxiety and/or irritability
- Up to 100-200 symptoms based on body system involvement
Currently, there is no single diagnostic test; however, there are set exclusionary accepted international criteria for diagnosis. Currently, there is no known cure. Management focuses on symptom relief, pacing, and supportive care. ME/CFS can last for years and ranges in severity from mild (limiting daily activities) to very severe (bed-bound and dependent on others for care).
Treatment
Treatment for ME/CFS is about managing symptoms and pain.
The key to symptom management is pacing.
If PEM (post-exertional malaise) is experienced, you must avoid exercise and activities that cause fatigue or increased symptoms and conserve your energy.
Long COVID
Long-COVID refers to a condition where symptoms persist or develop after the initial COVID-19 (SARS-CoV-2) infection, lasting beyond the expected recovery period. While most people recover from COVID-19 within a few weeks, some continue to experience ongoing and often disabling symptoms. This is sometimes called Post-COVID-19 Syndrome or “Long-COVID.”
The World Health Organization defines Long-COVID as symptoms that continue twelve weeks or more after infection and cannot be explained by another diagnosis.
Symptoms may include:
- Severe fatigue and exhaustion
- Post-exertional malaise (worsening of symptoms after activity)
- Cognitive difficulties (“brain fog”)
- Shortness of breath, chest pain, or heart palpitations
- Sleep problems
- Muscle and joint pain
- Autonomic issues such as dizziness or rapid heart rate (POTS/orthostatic intolerance)
- Sensory issues such as loss of taste or smell
- There are up to 200 symptoms based on body system involvement.
- A diagnosis of Long-COVID does not require the same degree of functional impairment (such as a 50% or greater reduction in physical and mental activity) that is required for a diagnosis of ME/CFS.
Prevention of Long-COVID
Prevention: After COVID-19, many people are eager to regain their health and return to normal life as quickly as possible. However, evidence shows that pushing too hard—whether physically or mentally—during the recovery phase can worsen symptoms, prolong recovery, or even lead to a diagnosis of ME/CFS. It is therefore vital to pace yourself and take exceptional care during this time. Some individuals may be genetically more vulnerable to post-viral illness, and those already living with ME/CFS are at particular risk of relapse if they over-exert. These insights highlight the importance of rest, gradual recovery, and self-compassion for anyone recovering from COVID-19.
Types of Long COVID
- Long-COVID (mixed symptoms): The largest group, experiencing a combination of symptoms directly related to COVID-19 (such as respiratory or cardiac problems) alongside symptoms that overlap with ME/CFS.
- Post-COVID ME/CFS: A smaller group whose illness is indistinguishable from ME/CFS, with no ongoing COVID-specific symptoms. This group develops ME/CFS following COVID-19.
- Long-COVID with COVID-only symptoms: A smaller group whose symptoms are only related to COVID-19 complications (e.g., lung scarring, clotting issues) and do not include ME/CFS features. As an ME/CFS support service, we do not support this group.
Occasionally, individuals may develop a chronic post-immune condition following vaccination, with symptoms overlapping those of ME/CFS. In such cases, this may be described as vaccine-triggered ME/CFS, rather than Long-COVID.
Progression
- Symptoms that last longer than twelve weeks after COVID-19 onset may be diagnosed as Long-COVID.
- If symptoms remain beyond eighteen months, particularly when ME/CFS features are dominant, a diagnosis of Post-COVID ME/CFS may be appropriate.
Treatment
Treatment for Long-COVID is similar to that of ME/CFS. It is about managing symptoms and pain.
The key to symptom management is pacing.
If PEM (post-exertional malaise) is experienced, you must avoid exercise and activities that cause fatigue or increased symptoms and conserve your energy.
The ME Association in the UK has developed a document to discuss whether ME and Long-COVID are the same condition: https://meassociation.org.uk/literature/items/long-covid-and-me-cfs-are-they-the-same-condition/
Fibromyalgia
Fibromyalgia is a chronic condition characterised by widespread musculoskeletal pain, fatigue, and heightened sensitivity to touch, pressure, or other stimuli. It affects the nervous system, altering the way the brain processes pain signals, and can lead to a variety of physical and cognitive symptoms.
The cause of Fibromyalgia is thought to involve a combination of genetic, neurological, and environmental factors, including previous infections, physical trauma, or emotional stress. It often occurs alongside other chronic conditions, including ME/CFS.
People with Fibromyalgia generally experience pain in specific points around the body. These points are no longer used to gauge for diagnosis; however, it is a helpful way of explaining where people are likely to feel pain.
(See https://www.healthline.com/health/fibromyalgia/fibromyalgia-tender-points for more information.)
The points around the body are:
- Back of the head
- Area between the shoulders
- Front of the neck
- Top of the chest
- Outside of the elbows
- Top and sides of the hips
- Insides of the knees
Typical features include:
- Widespread, persistent pain in muscles, ligaments, and joints
- Fatigue and low energy
- Sleep disturbances and unrefreshing sleep
- Cognitive difficulties, often called “fibro fog” (memory and concentration issues)
- Headaches or migraines
- Sensitivity to light, sound, temperature, or touch
- Irritable bowel symptoms or other digestive issues
- Mood changes, including anxiety or depression
Onset and course:
- Fibromyalgia can develop gradually over time or after a triggering event such as infection, injury, or significant stress.
- Symptoms fluctuate in severity, and flare-ups may be triggered by stress, physical activity, or environmental factors.
- Fibromyalgia is a long-term condition, and while there is currently no cure, management focuses on symptom relief, pacing, lifestyle adjustments, and supportive care.
Post-Viral Fatigue / Syndrome
Post-Viral Fatigue (sometimes called Post-Viral Fatigue Syndrome, PVFS) is a condition where fatigue and other symptoms continue well beyond the expected recovery time after a viral infection. In most straight-forward viral illnesses, recovery takes 2–4 weeks, with symptoms disappearing by six weeks. However, a small percentage of PVF/S patients may take several months to recover.
Typical features include:
- Persistent fatigue and lack of energy
- Reduced tolerance to activity (physical or mental)
- Poor concentration or “brain fog”
- Unrefreshing sleep
- Muscle aches or generalised pain
- Slower recovery from exertion
For many, PVF/S improves gradually over time as the body heals. If symptoms persist for at least six months in adults, or three months in children, and there is no significant improvement, the condition may be diagnosed as Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS).
Dysautonomia
Dysautonomia is a term for a group of diseases that include Postural Orthostatic Tachycardia Syndrome (POTS), Neurally Mediated Hypertension (“NMH”) and Orthostatic Intolerance (OI).
In these conditions, the autonomic nervous system (“ANS”) is dysregulated, which can lead to blood pressure problems, heart problems, trouble with breathing and swallowing, and erectile dysfunction in men.
Postural Orthostatic Tachycardia Syndrome (POTS)
Main symptoms include:
- Fatigue
- Headaches
- Light-headedness and dizziness
- An extreme increase in heart rate upon moving from a supine position to sitting position or standing position (extreme defined as over 100bpm). Diagnostic criteria involves if it rises by 30bpm in adults or 40bpm in youth, within 10 mins of standing. For most individuals living with POTS, this means experiencing an increase in heart rate above 100 to 200 compared to the expected heart rate of 60.
- Exercise intolerance
- Nausea
- Diminished concentration and forgetfulness
- Tremulousness (shaking)
- Coldness or pain in the extremities
- Excessive sweating
- Chest pain and shortness of breath.
- Sleep difficulties
- Anxiety (as an autonomic dysfunction)
Neurally Mediated Hypertension (“NMH”)
Abnormal reflex lowering of blood pressure during upright posture (low blood pressure created via the nervous system).
- Low blood pressure from faulty brain signals / ‘miscommunication’ between the heart and brain.
- Causes blood pressure to drop when a person has been standing for long periods, which is the opposite of what is needed, i.e. for the heart to beat faster to pump blood back up to the brain. Many people will not be able to “stand still” and they will walk to pump their legs in an attempt to push blood back up to the heart unconsciously.
- Leads to dizziness, nausea, and fainting.
Dr. Vallings refers to this as “3rd aisle of the supermarket;” after getting from the car to the supermarket and around a few aisles, fainting and falling becomes a possibility as there is a sudden feeling of the plug being pulled, marked by nausea, dizziness, fatigue, and brain fog.
Orthostatic Intolerance (“OI”)
POTS and NMH both have Orthostatic Intolerance as their primary symptom.
Orthostatic Intolerance is an umbrella term for the development of symptoms when in an upright posture.
OI can be caused by standing in an upright position for long periods of time, after being in a warm environment, immediately after exercise, after an emotionally stressful event, after eating (blood flow moved to digest food), or if salt and fluid intake is inadequate. These symptoms subside when returning to a horizontal position.
Symptoms of OI include:
- Light-headedness
- Altered vision
- Headache
- Heart palpations
- Exercise Intolerance
- Fatigue
- Neurocognitive deficits
- Anxiety
- Nausea
- Abdominal discomfort
- Tremulousness
- Sweating
- Weakness
- Syncope (fainting)
MISSION AND VISION
Complex Chronic Illness Support’s vision is to empower people towards wellness. our purpose is to improve the quality of life of people who live with a complex chronic illness, as well as that of their loved ones. With our support people with complex chronic illnesses can, in time, develop an increased ability to participate in family, social and community life, and lead a life that is fulfilling and meaningful for them.
Let’s talk
If you’d like to learn more about any of our services, or get involved, we’d love to hear from you.