Health Professional Referral
To refer your client to Complex Chronic Illness Support, please complete the secure form:
Chronic fatigue syndrome (CFS) is a complicated disorder characterised by extreme fatigue that lasts for at least six months and that can’t be fully explained by an underlying medical condition. The fatigue worsens with physical or mental activity but doesn’t improve with rest. There’s no single test to confirm a diagnosis of chronic fatigue syndrome and there is no known cure. You may need a variety of medical tests to rule out other health problems that have similar symptoms. Treatment for chronic fatigue syndrome focuses on improving symptoms.
Health Professionals are often the first to see people with ME/CFS and related disorders. CCI Support recognises this and understands that within your own limited resources it is impossible for Health Professionals to address all the aspects of care required for these complex cases. We would like to work together with Health Professionals to provide the holistic support and education required to patients and their Whanau.
CCI Support has a vision to “Empower People Towards Wellness” and our purpose is to improve the quality of life of
people who suffer from a complex chronic illness, as well as that of their loved ones.
Please note that CCI Support follows Internationally recognised Best Practice Guidelines for the treatment and management of energy-limiting conditions, such as ME/CFS, Long COVID and Fibromyalgia.
We provide support for long COVID, ME/CFS and Fibromyalgia.
We do have resource packs available for Health Professionals as well as extra brochures available for your clients.
Long COVID Registry
The University of Auckland has established a Long COVID registry, as part of an ongoing research project funded by the Ministry of Health via the COVID-19 and National Immunisation Programme Research Programme and the EuroQol Foundation. You can find out more information about it here: About the Long COVID registry

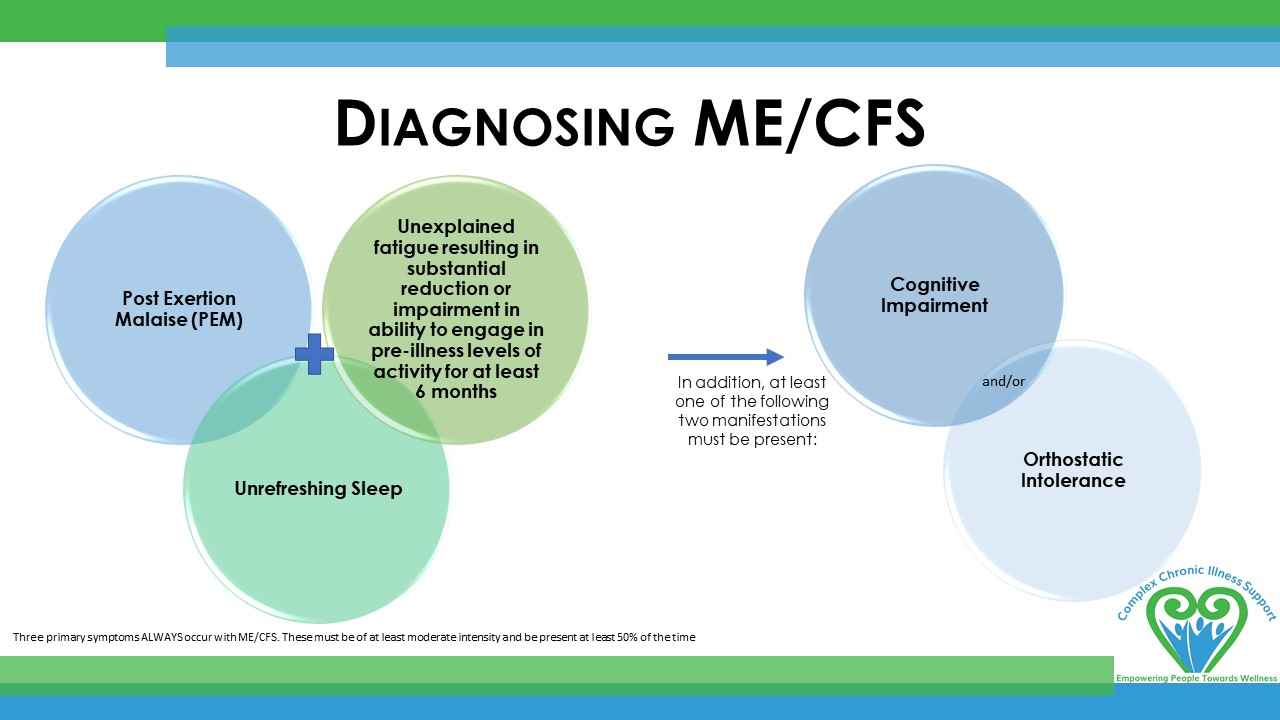
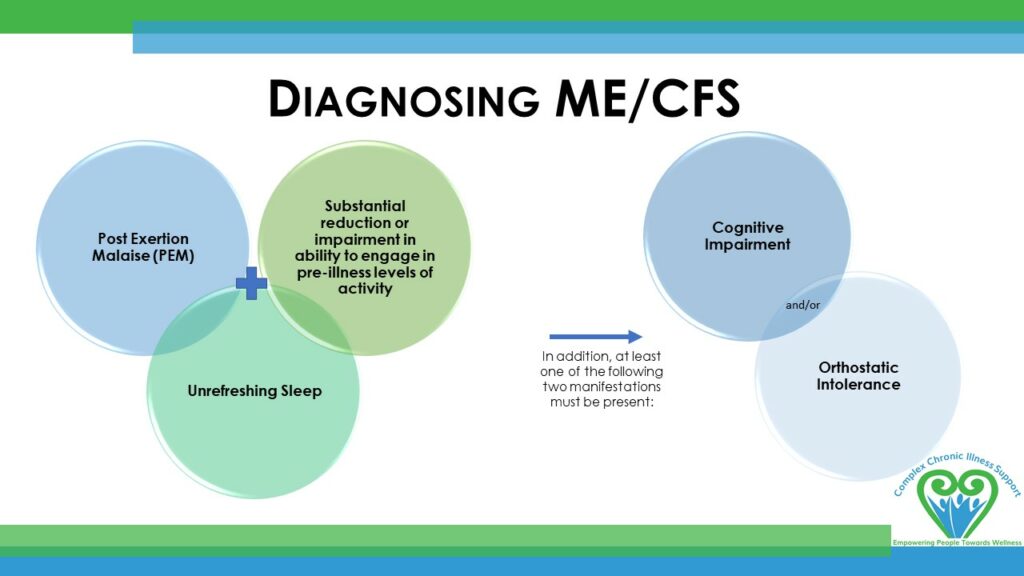
Diagnosing ME/CFS
Institute of Medicine (IoM) criteria
Three primary symptoms ALWAYS occur with ME/CFS. These must be of at least moderate intensity and be present at least 50% of the time to diagnose a patient with ME/CFS:
The diagnosis of ME/CFS is based on the patient’s history, pattern of symptoms, and the exclusion of other fatiguing illnesses. Clinical Primer Diagnostic Criteria Worksheet
The terms chronic fatigue syndrome and myalgic encephalomyelitis (ME/CFS) describe a complex physical illness characterized by debilitating fatigue, post-exertional malaise, pain, cognitive problems, sleep dysfunction and an array of other immune, neurological and autonomic symptoms. The key feature of the syndrome, post-exertional malaise, is the exacerbation of symptoms following minimal physical or mental activity, which can persist for hours, days or even weeks. Rest and sleep produce only modest relief of fatigue and the other symptoms. The illness is also characterized by substantially reduced physical and/or cognitive functioning. Although ME/CFS is a physical illness, secondary psychological symptoms may be present as in many other chronic illnesses.
Managing ME/CFS
The management of ME/CFS is as complex as the condition itself. CCI Support works in a holistic way with patients and families with ME/CFS, Fibromyalgia and related conditions. We understand the limitations within primary practice and aim to work WITH Health Professionals to provide well-rounded care.
- Manage the Symptoms
- We are happy to send you a resource pack with the latest information re: management of these conditions. ORDER HERE
- M.E. Awareness and Dr. Cathy Stephenson have collaborated in a GP presentation, it is well worth the time to watch this. WATCH HERE
- Treat Comorbidities
- Be aware of the contraindications
-
Graded exercise therapy (GET) is no longer recommended for ME/CFS.
-
Statement – CCIS Position on Graded Exercise Therapy
-
Statement ‘Global move away from ineffective therapies for ME/CFS’, 21 August 2021
Emeritus Professor Warren Tate, Biochemistry, University of Otago -
Statement ‘ME/CFS and Exercise’, 2 September 2021
Dr. Lynette Hodges, Senior Lecturer in Sport and Exercise, Massey University -
The NICE Guidelines cover diagnosing and managing myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome (ME/CFS) in children, young people and adults.
-
Cognitive behavioural therapy, CBT, is no longer recommended as a treatment for ME/CFS
-
- The patient may require:
- Disability Allowance to cover their costs
- They may benefit from being on Support Living Payments instead of a Job Seekers benefit
- A referral to NASC for home help
- Specialist referrals to sleep specialist, local pain clinic, rheumatologist for Fibromyalgia etc
- A pamphlet from CCIS, explaining how they can access our services
- CCI Support has the expertise to provide support and education around:
- Understanding the Condition
- Pacing – Balancing Activity & Rest
- Stress Management
- Understanding pain
- Nutrition / Gut Health
- Restorative Movement
- Sleep
- Building and maintaining a Support Network
- Counselling in some regions
- Low Level Advocacy re: employment options, WINZ and other government agencies
From Harm to Help
Promoting an evidence-based shift in our understanding of Myalgic Encephalomyelitis / Chronic Fatigue Syndrome
Presentation by Dr. Cathy Stephenson, RNZCGP General Practice Conference, 7th August 2021
In collaboration with M.E. Awareness NZ
ANZMES CME education for Health Professionals
Know M.E the video podcast and news series: sharing the latest medical research and up-to-date, relevant information to help clinicians, researchers and other health professionals stay informed about this challenging and often misunderstood condition: Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and post COVID conditions.
ANZMES is a RNZCGP registered provider of continuing education. Earn credits while you learn.
RNZCGP accredited CME (Continuing Medical Education)
M.E. Awareness has a comprehensive list of CME sessions available, including:
NZ Doctor (8th April 2020) ‘How to Treat’ article on Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome
Pages 25-29 – 1 RNZCGP credit M.E. Awareness | How to Treat ME/CFS
ThinkGP – Module 1 (Australia, 2021) “Busting the myths and redefining myalgic encephalomyelitis /chronic fatigue syndrome (ME/CFS)”
Module 1. View our brief introduction to this RNZCGP-endorsed CME here. 1 RNZCGP credit
ThinkGP – Module 2 (Australia, 2021) “Ensuring a patient-centred approach to care for people living with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)”.
International Continuing Medical Education
Myalgic Encephalomyelitis / Chronic Fatigue Syndrome CPD, 10 clinical cases, StudyPRN (UK, May 2020)
Unrest CME (USA, Nov 2018)
International Continuing Medical Education
A good link for Physios is Physios for ME
NASA 10 minute Lean Test
The Bateman Horne Center recommends that all ME/CFS and Fibromyalgia patients have a NASA 10-minute Lean Test to assess for orthostatic intolerance.
Recently we created a PowerPoint presentation to explain CCI Support Services to Health Professionals.
CME/CNE session with Dr Ros Vallings - July 2021
This CME/CNE education session will assist attendees to further understand the condition and latest research; diagnosis efficacy and effective management, along with complex chronic illness support services, and how to refer.
Illnesses We Support
Myalgic Encephalomyelitis (ME) / Chronic Fatigue Syndrome
Myalgic Encephalomyelitis (ME) also known as chronic fatigue syndrome (CFS) - an abnormal immune system response to any number of infectious or environmental triggers, causing a long-term illness that can result in significant disability.
The main symptoms include
- persistent and overwhelming fatigue
- post-exertional malaise
- muscle and/or joint pains
- cognitive dysfunction
- sleep disturbance
- digestive problems
It is estimated that there are between 16 000 to 20 000 people with ME/CFS effecting people of all ages, ethnicity, and socio-economic groups, although there is higher prevalence among women than men. ME/CFS is challenging to diagnosis in which other conditions need to be ruled out and a specific set of diagnostic criteria met. There are currently no specific medical treatments for ME/CFS.
Symptom severity ranges from ‘mild’ (just able to manage work but at the expense of other areas of life), to ‘very severe’ (bed-bound, tube-fed, paralysed, without speech). Even symptoms which are classed as mild can involve the loss of at least 50% of normal function.
Fibromyalgia
A chronic condition causing fatigue, widespread pain, and tenderness throughout the body and often co-exists with ME/CFS and/or many of the symptoms of this condition. People with Fibromyalgia generally experience pain in specific points around the body and these points are used as a gauge for diagnosis.
Fibromyalgia is a syndrome rather than a disease. Unlike a disease, which is a medical condition with a specific cause or causes and recognizable signs and symptoms, a syndrome is a collection of signs, symptoms, and medical problems that tend to occur together but are not related to a specific, identifiable cause.
For those with severe symptoms, fibromyalgia can be extremely debilitating and interfere with basic daily activities. Fibromyalgia affects two to four % of the population, mainly women, although men and adolescents can also develop the condition.
Symptoms:
- Chronic Widespread Pain
- Moderate to extreme incapacitating fatigue
- Sleep Disturbances
- Cognitive Difficulties
- Headaches
- Sensitivity to touch/light/sound
- Anxiety and/or depression
- Impaired coordination / balance
- Gastrointestinal problems
- Chemical senstivities
- Orthostatic intolerance
Post-Viral Fatigue / Syndrome
In most straight-forward viral illnesses, recovery takes 2-4 weeks, with symptoms disappearing by six weeks. However, in a small percentage of patients the duration until recovery can take up to several months. If symptoms remain after 3-6 months with the illness unchanged, a change of name/diagnosis to CFS/ME is appropriate.
Dysautonomia
Dysautonomia is a term used to describe autonomic nervous system dysfunction. Our autonomic nervous system acts largely unconsciously and regulates body functions.
A common form of Dysautonomia for people with ME/CFS is Orthostatic Intolerance, which is often caused by Neurally Mediated Hypotension (NMH) or Postural Orthostatic Tachycardia Syndrome (POTS).
CCI Support only supports a few Dysautonomia conditions; Postural Orthostatic Tachycardia Syndrome (POTS) and Neurally Mediated Hypotension (NMH).
Long COVID
Long COVID is a term used to describe the symptoms that continue or develop after your initial COVID-19 illness and cannot be explained by any other condition. Long COVID is usually diagnosed when symptoms continue more than 3 months after the initial COVID-19 diagnosis.
For some people, corona virus disease 2019 (COVID-19) can cause symptoms that last weeks or months after the infection has gone. This is sometimes called post-COVID-19 syndrome or “long COVID”.
Research from Professor Tate states that people who develop Long COVID develop a chronic inflammatory immune response in the body system. This has strong neurological symptoms like brain fog and sleep dysfunctions. Inflammation in the brain is called neuro inflammation. The brain is misfunctioning and communicating back to the body that it is in danger and the inflammatory response just keeps going, resulting in a vicious cycle and on-going disease.
Both Myalgic Encephalomylitis (ME/CFS) and Long COVID share certain key symptoms and may exhibit a comparable degree of fluctuating functional impairment. Nevertheless, there are significant distinctions that set apart individuals with Long Covid from those with ME/CFS
There seems to be 3 very distinct variations of Long COVID:
- A significant amount of people are presenting with symptoms directly related to COVID with ME symptoms too
- Some people are presenting with ME symptoms and no COVID symptoms - labelled Post-Covid ME/CFS
- A smaller group of people with COVID symptoms ONLY - These people are best treated/managed directly within the medical system.
- We are also seeing a considerable amount of people with a ME/CFS history, relapsing with ME/CFS after getting COVID-19
COVID Symptoms - A considerable portion of individuals with Long Covid experience an additional layer of symptoms directly linked to the involvement of various organs such as lungs, heart, blood vessels, liver, kidneys, brain, nervous system, gastrointestinal tract, or skin. These symptoms typically stem from damage or disruption in the function of these organs during the initial infection. Common Covid-specific symptoms include*:
- Shortness of breath and/or cough
- Chest pains
- Cardiac arrhythmias or heart-rhythm disturbances
- Palpitations upon exertion
- Periodic fevers
- Loss or alteration of taste (parosmia) and/or smell
- Abdominal pain and diarrhea, which may indicate post-Covid irritable bowel syndrome or an inflammatory bowel syndrome
- Skin rashes, including phenomena like 'Covid toe'
- Hair loss
A diagnosis of Long Covid does not require the presence of the very significant (ie 50% or more) functional impairment relating to physical and mental activity that is required to confirm a diagnosis of ME/CFS.
Treatment for Long COVID is similar to that of ME/CFS. It is about managing symptoms and pain.
The key to symptom management is pacing.
If PEM (post-exertional malaise) is experienced, you must avoid exercise and activities that cause fatigue or increased symptoms, and conserve your energy.
* https://meassociation.org.uk/literature/items/long-covid-and-me-cfs-are-they-the-same-condition/
How CCIS Supports Clients
Primers and Diagnostic Tools
ME/CFS Primer
This primer was developed by consensus among members of the primer committee for use by clinical practitioners. The primer provides information essential to understanding, diagnosing and managing the symptoms of Myalgic Encephalomyelitis (ME) otherwise known as Chronic Fatigue Syndrome (CFS)
Fibromyalgia Diagnostic Criteria
AAPT Diagnostic Criteria for Fibromyalgia
The International Fibromyalgia working group diagnostic criteria adopted by ACTTION-APS Pain Taxonomy (AAPT)
ME/CFS Pediatric Primer
This primer was written by the International Writing Group for Pediatric ME/CFS. The primer provides information essential to understanding, diagnosing and managing the symptoms of Myalgic Encephalomyelitis (ME) otherwise known as Chronic Fatigue Syndrome (CFS) in children and adolescents.
Orthostatic Intolerance
Orthostatic Intolerance & it’s treatment
General Information Brochure on Orthostatic Intolerance and its Treatment by Peter C. Rowe, MD, Chronic Fatigue Clinic at the Johns Hopkins Children Center
POTS Diagnostics
Current diagnostic criteria and management of Postural Orthostatic Tachycardia Syndrome.
Fedorowski, A. (2018). Postural orthostatic tachycardia syndrome: Clinical presentation, aetiology and management. Journal of International Medicine, 285(4), 352-366.
POTS Diagnostics
A handy 1 page guide to POTS for Health Professionals
Author: Prof Lesley Kavi, Published 19/04/2020 potsuk.org
EXTRA RESOURCES...
CCI Support has been following research from around the world for over 4 decades. This link will take you to what we feel is some of the most reputable sites for information of Chronic Fatigue Syndrome and related disorders.
Medical Research
As an agency, we like to keep up to date with the research going on around the world. Here are some articles of interest.
Unveiling the Link between Tick-Borne Illness and Post viral Fatigue
Unveiling the Link between Tick-Borne Illness and Post viral Fatigue: Insights from Crimean-Congo Haemorrhagic Fever Study Introduction: In an unexpected turn, a recent study delves into the post viral effects of Crimean-Congo Haemorrhagic Fever Virus (CCHFV) on...
Elevated blood lactate in resting conditions
Research Article: Elevated blood lactate in resting conditions correlate with post exertional malaise severity in patients with Myalgic encephalomyelitis/Chronic Fatigue Syndrome. The study looked into the phenomenon of elevated blood lactate levels at rest among...
Caring for the Patient with Severe or Very Severe Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
This article is an excellent introduction to the unique challenges of severe or very severe ME/CFS. It covers the symptoms and pathology, the specialised care that is required from healthcare providers, common misunderstandings around severe M.E. (i.e., that it is...
A Science-Supported Journaling Protocol to Improve Mental & Physical Health
A lot of people report that Journaling has been a big part of their health improvement. Here is a Specific writing protocol shown in hundreds of scientific studies to significantly improve immediate and long-term health. It explains how to implement this specific...
The role of sleep and dreams in long-COVID
While it is well known that sleep disturbances are a common symptom for those with Long COVID, there has been little research into the different types of sleep disturbances that are experienced. The research paper the role of sleep and dreams in long-COVID...
Helen Clark Foundation – Long COVID – are we taking it seriously enough
Post-meeting recording can be found here: Long Covid - are we taking it seriously enough? Wednesday 3 April, 12pm-1.15pm Join us for an expert discussion on long Covid. As the public focus on Covid-19 has waned and the public has largely returned to...
Immunological Patient Stratification in ME / CFS
If this article is too long for your energy levels, please see at the bottom for a quick summary. You have probably heard us tell you that different treatments will work for different people. What works for one of you might not be so helpful for another. There are...
NMLS: Study identifies mitochondrial dysfunction as cause of long-COVID fatigue
Researchers from Amsterdam UMC and Vrije Universiteit Amsterdam (VU) have discovered that the persistent fatigue in patients with long-COVID has a biological cause, namely mitochondria in muscle cells that produce less energy than in healthy patients. "We saw various...
NPR: A discovery in the muscles of long COVID patients may explain exercise troubles
The original article can be found here: https://www.npr.org/sections/health-shots/2024/01/09/1223077307/long-covid-exercise-post-exertional-malaise-mitochondria Please note only snippets of the article are included below. Please follow the link to read the full...
Friendly Gut Bacteria Speeds Long-COVID Recovery
A year long investigation was undertaken in the UK which has resulted in a research paper concluding that using a concoction of lactobacillus probiotics in combination with chicory containing inulin may help to reduce symptoms of COVID and Long-COVID. Inulin is a prebiotic which feeds healthy bacteria in the gut. Chicory contains a high amount of inulin.
Let’s talk
If you’d like to learn more about any of our services, or get involved, we’d love to hear from you.