Health Professional Referral
To refer your client to Complex Chronic Illness Support, please complete the secure form:
Myalgic Encephalomyelitis/Chronic fatigue syndrome (ME/CFS) is a complicated disorder characterised by extreme fatigue that lasts for at least six months and that can’t be fully explained by an underlying medical condition. The fatigue worsens with physical or mental activity but doesn’t improve with rest. There’s no single test to confirm a diagnosis of ME/CFS and there is no known cure. A person may need a variety of medical tests to rule out other health problems that have similar symptoms. Treatment for ME/CFS focuses on improving symptoms.
Health Professionals are often the first to see people with ME/CFS and related disorders. CCI Support recognises this and understands that within your own limited resources it is impossible for Health Professionals to address all the aspects of care required for these complex cases. We would like to work together with Health Professionals to provide the holistic support and education required to patients and their Whanau.
CCI Support has a vision to “Empower People Towards Wellness” and our purpose is to improve the quality of life of
people who suffer from a complex chronic illness, as well as that of their loved ones.
We provide support for long COVID, ME/CFS and Fibromyalgia.
We do have resource packs available for Health Professionals as well as extra brochures available for your clients.
Long COVID Registry
The University of Auckland has established a Long COVID registry, as part of an ongoing research project funded by the Ministry of Health via the COVID-19 and National Immunisation Programme Research Programme and the EuroQol Foundation. You can find out more information about it here: About the Long COVID registry

Please note that CCI Support Stands with International Best Practice for ME/CFS & Long COVID.
At CCI Support, we align with international best practice guidelines for the management of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and Long COVID. We do not support the use of Graded Exercise Therapy (GET) or Cognitive Behavioural Therapy (CBT) as primary treatments, as these approaches have been shown to cause harm.
For decades, GET and CBT were promoted by a small group of psychiatrists under the belief that ME/CFS was a disorder of perception. However, extensive research now confirms that exertion worsens symptoms—what we now recognise as Post-Exertional Malaise (PEM).
The global shift away from these outdated therapies follows key reports, including:
📌 The 2015 Institute of Medicine (now National Academy of Medicine, USA) report, which affirmed that ME/CFS is a serious biomedical illness requiring urgent attention.
📌 The 2020 National Institute for Health and Care Excellence (NICE, UK) review, which reinforced that GET and CBT are not appropriate treatments.
As research evolves, so must healthcare practices. CCI Support remains committed to evidence-based, compassionate care that prioritises the well-being of those living with ME/CFS and Long COVID.
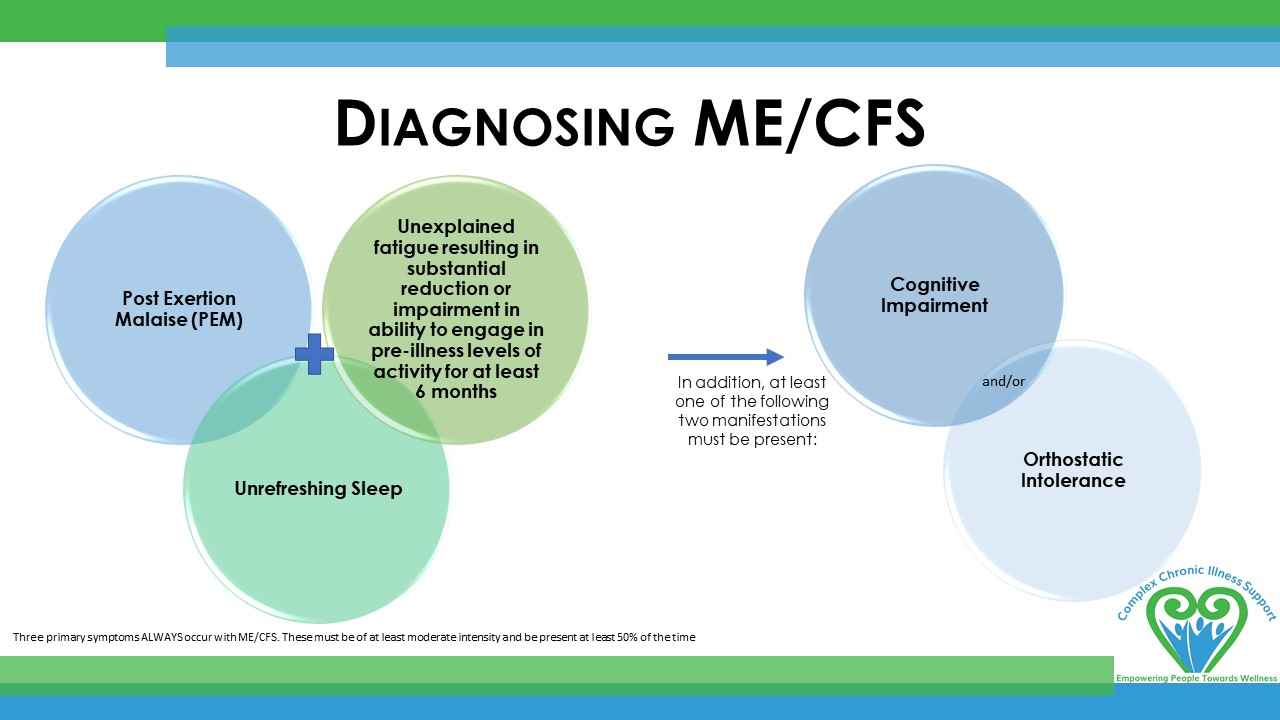
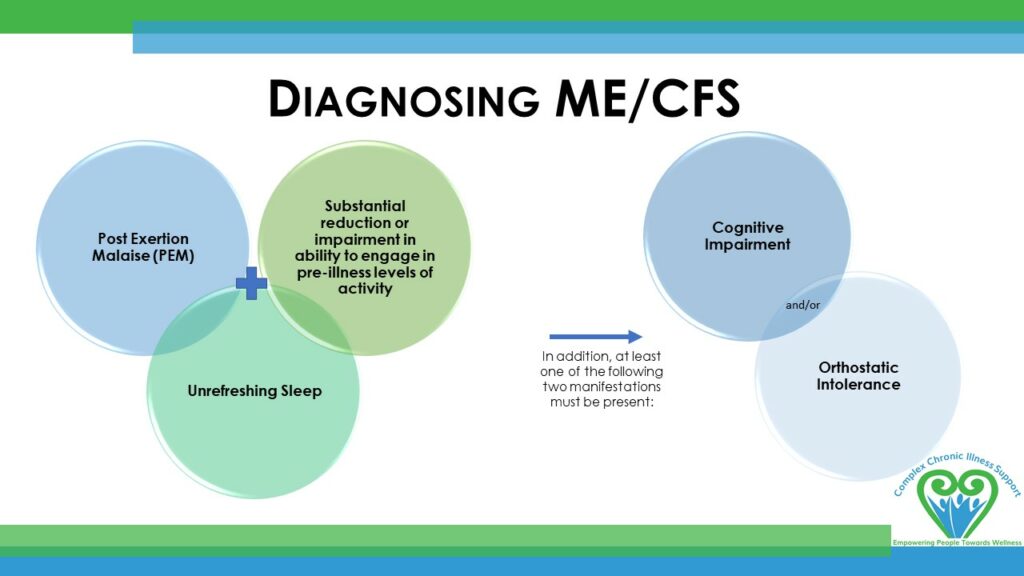
Diagnosing ME/CFS
Institute of Medicine (IoM) criteria
Three primary symptoms ALWAYS occur with ME/CFS. These must be of at least moderate intensity and be present at least 50% of the time to diagnose a patient with ME/CFS:
The diagnosis of ME/CFS is based on the patient’s history, pattern of symptoms, and the exclusion of other fatiguing illnesses. Clinical Primer Diagnostic Criteria Worksheet
The terms chronic fatigue syndrome and myalgic encephalomyelitis (ME/CFS) describe a complex physical illness characterised by debilitating fatigue, post-exertional malaise, pain, cognitive problems, sleep dysfunction and an array of other immune, neurological and autonomic symptoms. The key feature of the syndrome, post-exertional malaise, is the exacerbation of symptoms following minimal physical or mental activity, which can persist for hours, days or even weeks. Rest and sleep produce only modest relief of fatigue and the other symptoms. The illness is also characterised by substantially reduced physical and/or cognitive functioning. Although ME/CFS is a physical illness, secondary psychological symptoms may be present as in many other chronic illnesses.
Managing ME/CFS
The management of ME/CFS is as complex as the condition itself. CCI Support works in a holistic way with patients and families with ME/CFS, Fibromyalgia and related conditions. We understand the limitations within primary practice and aim to work WITH Health Professionals to provide well-rounded care.
- Manage the Symptoms
- We are happy to send you a resource pack with the latest information re: management of these conditions. ORDER HERE
- M.E. Awareness and Dr. Cathy Stephenson have collaborated in a GP presentation, it is well worth the time to watch this. WATCH HERE
- Treat Comorbidities
- Be aware of the contraindications
-
Graded exercise therapy (GET) is no longer recommended for ME/CFS.
-
Statement – CCIS Position on Graded Exercise Therapy
-
Statement ‘Global move away from ineffective therapies for ME/CFS’, 21 August 2021
Emeritus Professor Warren Tate, Biochemistry, University of Otago -
Statement ‘ME/CFS and Exercise’, 2 September 2021
Dr. Lynette Hodges, Senior Lecturer in Sport and Exercise, Massey University -
The NICE Guidelines cover diagnosing and managing myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome (ME/CFS) in children, young people and adults.
-
Cognitive behavioural therapy, CBT, is no longer recommended as a treatment for ME/CFS
-
- The patient may require:
- Disability Allowance to cover their costs
- They may benefit from being on Support Living Payments instead of a Job Seekers benefit
- A referral to NASC for home help
- Specialist referrals to sleep specialist, local pain clinic, rheumatologist for Fibromyalgia etc
- A pamphlet from CCIS, explaining how they can access our services
- CCI Support has the expertise to provide support and education around:
- Understanding the Condition
- Pacing – Balancing Activity & Rest
- Stress Management
- Understanding pain
- Nutrition / Gut Health
- Restorative Movement
- Sleep
- Building and maintaining a Support Network
- Counselling in some regions
- Low Level Advocacy re: employment options, WINZ and other government agencies
From Harm to Help
Promoting an evidence-based shift in our understanding of Myalgic Encephalomyelitis / Chronic Fatigue Syndrome
Presentation by Dr. Cathy Stephenson, RNZCGP General Practice Conference, 7th August 2021
In collaboration with M.E. Awareness NZ
ANZMES CME education for Health Professionals
Know M.E the video podcast and news series: sharing the latest medical research and up-to-date, relevant information to help clinicians, researchers and other health professionals stay informed about this challenging and often misunderstood condition: Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and post COVID conditions.
ANZMES is a RNZCGP registered provider of continuing education. Earn credits while you learn.
RNZCGP accredited CME (Continuing Medical Education)
M.E. Awareness has a comprehensive list of CME sessions available, including:
NZ Doctor (8th April 2020) ‘How to Treat’ article on Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome
Pages 25-29 – 1 RNZCGP credit M.E. Awareness | How to Treat ME/CFS
ThinkGP – Module 1 (Australia, 2021) “Busting the myths and redefining myalgic encephalomyelitis /chronic fatigue syndrome (ME/CFS)”
Module 1. View our brief introduction to this RNZCGP-endorsed CME here. 1 RNZCGP credit
ThinkGP – Module 2 (Australia, 2021) “Ensuring a patient-centred approach to care for people living with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)”.
International Continuing Medical Education
Myalgic Encephalomyelitis / Chronic Fatigue Syndrome CPD, 10 clinical cases, StudyPRN (UK, May 2020)
Unrest CME (USA, Nov 2018)
International Continuing Medical Education
A good link for Physios is Physios for ME
NASA 10 minute Lean Test
The Bateman Horne Center recommends that all ME/CFS and Fibromyalgia patients have a NASA 10-minute Lean Test to assess for orthostatic intolerance.
CME/CNE session with Dr Ros Vallings - July 2021
This CME/CNE education session will assist attendees to further understand the condition and latest research; diagnosis efficacy and effective management, along with complex chronic illness support services, and how to refer.
Illnesses We Support
Myalgic Encephalomyelitis (ME) / Chronic Fatigue Syndrome
Myalgic Encephalomyelitis, also known as Chronic Fatigue Syndrome (together referred to as ME/CFS), is a debilitating, long-term, multi-system illness. It can affect the immune, neurological, endocrine, and autonomic systems, leading to a wide range of confusing and disabling symptoms. It has been described as an abnormal immune system response to any number of infectious or environmental triggers, causing a long-term illness that can result in significant disability.
Known triggers are viral infection, or a myriad of triggers, including but not limited to adverse/allergic reactions to anaesthesia/vaccination, chemical toxicity, hormonal fluctuations (childbirth, menopause), physical/emotional trauma, and/or genetic predisposition. There is also emerging research to show genetic links.
Approximately 80% of cases are preceded by a viral infection, such as:
- Common cold
- Influenza
- Pneumonia
- Epstein-Barr virus/Glandular fever
- Herpes virus
- COVID-19
While many people recover from viral illness within a few weeks, those with ME/CFS do not return to full health and instead develop persistent, life-altering symptoms lasting at least six months prior to diagnosis for adults, and three months for children.
In the case of COVID-19, symptoms lasting beyond twelve weeks may be diagnosed as Long-COVID, and if they persist beyond two years, they may be considered Long-COVID–induced ME/CFS.
People who have compromised/weakened immunity or have pre-existing conditions may be more prone to ME/CFS. At present, there are few treatment options available for ME/CFS.
- Onset: Can be triggered by a viral infection, but it can also have a gradual onset without a clear viral trigger.
- Symptoms: Prolonged and severe fatigue, often accompanied by cognitive dysfunction (brain fog), unrefreshing sleep, and pain. The symptoms are not solely explained by ongoing viral activity or other medical conditions.
- Duration: ME/CFS is characterised by persistent symptoms that last for at least six months. The severity of symptoms can fluctuate, but the condition is chronic, lasting for years.
It's important to note that while post-viral fatigue can resolve on its own as the body recovers from the initial infection, ME/CFS is considered a chronic condition with a more persistent and often disabling course. The defining diagnostic characteristic of ME/CFS is post-exertional malaise (PEM) – a worsening of symptoms after even small amounts of physical, mental, or emotional effort, often delayed by 24–72 hours.
Main symptoms include:
- PEM
- Unrefreshing sleep
- Unrelenting fatigue that cannot be explained by other conditions
- and then 1 of: Orthostatic intolerance or cognitive impairment – impaired memory and concentration.
- Muscle and/or joint pains
- Sleep disturbance
- Digestive problems
- Sensitivities to light and sound
- Headaches/migraines
- Sore throat and/or enlarged lymph nodes
- Dysregulated temperature control – fever/chills
- POTS
- Orthostatic intolerance – erratic heart rate, feeling faint or dizzy upon standing
- Anxiety and/or irritability
- Up to 100-200 symptoms based on body system involvement
Currently, there is no single diagnostic test; however, there are set exclusionary accepted international criteria for diagnosis. Currently, there is no known cure. Management focuses on symptom relief, pacing, and supportive care. ME/CFS can last for years and ranges in severity from mild (limiting daily activities) to very severe (bed-bound and dependent on others for care).
Treatment
Treatment for ME/CFS is about managing symptoms and pain.
The key to symptom management is pacing.
If PEM (post-exertional malaise) is experienced, you must avoid exercise and activities that cause fatigue or increased symptoms and conserve your energy.
Long COVID
Long-COVID refers to a condition where symptoms persist or develop after the initial COVID-19 (SARS-CoV-2) infection, lasting beyond the expected recovery period. While most people recover from COVID-19 within a few weeks, some continue to experience ongoing and often disabling symptoms. This is sometimes called Post-COVID-19 Syndrome or “Long-COVID.”
The World Health Organization defines Long-COVID as symptoms that continue twelve weeks or more after infection and cannot be explained by another diagnosis.
Symptoms may include:
- Severe fatigue and exhaustion
- Post-exertional malaise (worsening of symptoms after activity)
- Cognitive difficulties (“brain fog”)
- Shortness of breath, chest pain, or heart palpitations
- Sleep problems
- Muscle and joint pain
- Autonomic issues such as dizziness or rapid heart rate (POTS/orthostatic intolerance)
- Sensory issues such as loss of taste or smell
- There are up to 200 symptoms based on body system involvement.
- A diagnosis of Long-COVID does not require the same degree of functional impairment (such as a 50% or greater reduction in physical and mental activity) that is required for a diagnosis of ME/CFS.
Prevention of Long-COVID
Prevention: After COVID-19, many people are eager to regain their health and return to normal life as quickly as possible. However, evidence shows that pushing too hard—whether physically or mentally—during the recovery phase can worsen symptoms, prolong recovery, or even lead to a diagnosis of ME/CFS. It is therefore vital to pace yourself and take exceptional care during this time. Some individuals may be genetically more vulnerable to post-viral illness, and those already living with ME/CFS are at particular risk of relapse if they over-exert. These insights highlight the importance of rest, gradual recovery, and self-compassion for anyone recovering from COVID-19.
Types of Long COVID
- Long-COVID (mixed symptoms): The largest group, experiencing a combination of symptoms directly related to COVID-19 (such as respiratory or cardiac problems) alongside symptoms that overlap with ME/CFS.
- Post-COVID ME/CFS: A smaller group whose illness is indistinguishable from ME/CFS, with no ongoing COVID-specific symptoms. This group develops ME/CFS following COVID-19.
- Long-COVID with COVID-only symptoms: A smaller group whose symptoms are only related to COVID-19 complications (e.g., lung scarring, clotting issues) and do not include ME/CFS features. As an ME/CFS support service, we do not support this group.
Occasionally, individuals may develop a chronic post-immune condition following vaccination, with symptoms overlapping those of ME/CFS. In such cases, this may be described as vaccine-triggered ME/CFS, rather than Long-COVID.
Progression
- Symptoms that last longer than twelve weeks after COVID-19 onset may be diagnosed as Long-COVID.
- If symptoms remain beyond eighteen months, particularly when ME/CFS features are dominant, a diagnosis of Post-COVID ME/CFS may be appropriate.
Treatment
Treatment for Long-COVID is similar to that of ME/CFS. It is about managing symptoms and pain.
The key to symptom management is pacing.
If PEM (post-exertional malaise) is experienced, you must avoid exercise and activities that cause fatigue or increased symptoms and conserve your energy.
The ME Association in the UK has developed a document to discuss whether ME and Long-COVID are the same condition: https://meassociation.org.uk/literature/items/long-covid-and-me-cfs-are-they-the-same-condition/
Fibromyalgia
Fibromyalgia is a chronic condition characterised by widespread musculoskeletal pain, fatigue, and heightened sensitivity to touch, pressure, or other stimuli. It affects the nervous system, altering the way the brain processes pain signals, and can lead to a variety of physical and cognitive symptoms.
The cause of Fibromyalgia is thought to involve a combination of genetic, neurological, and environmental factors, including previous infections, physical trauma, or emotional stress. It often occurs alongside other chronic conditions, including ME/CFS.
People with Fibromyalgia generally experience pain in specific points around the body. These points are no longer used to gauge for diagnosis; however, it is a helpful way of explaining where people are likely to feel pain.
(See https://www.healthline.com/health/fibromyalgia/fibromyalgia-tender-points for more information.)
The points around the body are:
- Back of the head
- Area between the shoulders
- Front of the neck
- Top of the chest
- Outside of the elbows
- Top and sides of the hips
- Insides of the knees
Typical features include:
- Widespread, persistent pain in muscles, ligaments, and joints
- Fatigue and low energy
- Sleep disturbances and unrefreshing sleep
- Cognitive difficulties, often called “fibro fog” (memory and concentration issues)
- Headaches or migraines
- Sensitivity to light, sound, temperature, or touch
- Irritable bowel symptoms or other digestive issues
- Mood changes, including anxiety or depression
Onset and course:
- Fibromyalgia can develop gradually over time or after a triggering event such as infection, injury, or significant stress.
- Symptoms fluctuate in severity, and flare-ups may be triggered by stress, physical activity, or environmental factors.
- Fibromyalgia is a long-term condition, and while there is currently no cure, management focuses on symptom relief, pacing, lifestyle adjustments, and supportive care.
Post-Viral Fatigue / Syndrome
Post-Viral Fatigue (sometimes called Post-Viral Fatigue Syndrome, PVFS) is a condition where fatigue and other symptoms continue well beyond the expected recovery time after a viral infection. In most straight-forward viral illnesses, recovery takes 2–4 weeks, with symptoms disappearing by six weeks. However, a small percentage of PVF/S patients may take several months to recover.
Typical features include:
- Persistent fatigue and lack of energy
- Reduced tolerance to activity (physical or mental)
- Poor concentration or “brain fog”
- Unrefreshing sleep
- Muscle aches or generalised pain
- Slower recovery from exertion
For many, PVF/S improves gradually over time as the body heals. If symptoms persist for at least six months in adults, or three months in children, and there is no significant improvement, the condition may be diagnosed as Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS).
Dysautonomia
Dysautonomia is a term for a group of diseases that include Postural Orthostatic Tachycardia Syndrome (POTS), Neurally Mediated Hypertension (“NMH”) and Orthostatic Intolerance (OI).
In these conditions, the autonomic nervous system (“ANS”) is dysregulated, which can lead to blood pressure problems, heart problems, trouble with breathing and swallowing, and erectile dysfunction in men.
Postural Orthostatic Tachycardia Syndrome (POTS)
Main symptoms include:
- Fatigue
- Headaches
- Light-headedness and dizziness
- An extreme increase in heart rate upon moving from a supine position to sitting position or standing position (extreme defined as over 100bpm). Diagnostic criteria involves if it rises by 30bpm in adults or 40bpm in youth, within 10 mins of standing. For most individuals living with POTS, this means experiencing an increase in heart rate above 100 to 200 compared to the expected heart rate of 60.
- Exercise intolerance
- Nausea
- Diminished concentration and forgetfulness
- Tremulousness (shaking)
- Coldness or pain in the extremities
- Excessive sweating
- Chest pain and shortness of breath.
- Sleep difficulties
- Anxiety (as an autonomic dysfunction)
Neurally Mediated Hypertension (“NMH”)
Abnormal reflex lowering of blood pressure during upright posture (low blood pressure created via the nervous system).
- Low blood pressure from faulty brain signals / ‘miscommunication’ between the heart and brain.
- Causes blood pressure to drop when a person has been standing for long periods, which is the opposite of what is needed, i.e. for the heart to beat faster to pump blood back up to the brain. Many people will not be able to “stand still” and they will walk to pump their legs in an attempt to push blood back up to the heart unconsciously.
- Leads to dizziness, nausea, and fainting.
Dr. Vallings refers to this as “3rd Isle of the Supermarket;” after getting from the car to the supermarket and around a few aisles, fainting and falling becomes a possibility as there is a sudden feeling of the plug being pulled, marked by nausea, dizziness, fatigue, and brain fog.
Orthostatic Intolerance (“OI”)
POTS and NMH both have Orthostatic Intolerance as their primary symptom.
Orthostatic Intolerance is an umbrella term for the development of symptoms when in an upright posture.
OI can be caused by standing in an upright position for long periods of time, after being in a warm environment, immediately after exercise, after an emotionally stressful event, after eating (blood flow moved to digest food), or if salt and fluid intake is inadequate. These symptoms subside when returning to a horizontal position.
Symptoms of OI include:
- Light-headedness
- Altered vision
- Headache
- Heart palpations
- Exercise Intolerance
- Fatigue
- Neurocognitive deficits
- Anxiety
- Nausea
- Abdominal discomfort
- Tremulousness
- Sweating
- Weakness
- Syncope (fainting)
How CCIS Supports Clients
Primers and Diagnostic Tools
ME/CFS Primer
This primer was developed by consensus among members of the primer committee for use by clinical practitioners. The primer provides information essential to understanding, diagnosing and managing the symptoms of Myalgic Encephalomyelitis (ME) otherwise known as Chronic Fatigue Syndrome (CFS)
Fibromyalgia Diagnostic Criteria
AAPT Diagnostic Criteria for Fibromyalgia
The International Fibromyalgia working group diagnostic criteria adopted by ACTTION-APS Pain Taxonomy (AAPT)
ME/CFS Pediatric Primer
This primer was written by the International Writing Group for Pediatric ME/CFS. The primer provides information essential to understanding, diagnosing and managing the symptoms of Myalgic Encephalomyelitis (ME) otherwise known as Chronic Fatigue Syndrome (CFS) in children and adolescents.
Orthostatic Intolerance
Orthostatic Intolerance & it’s treatment
General Information Brochure on Orthostatic Intolerance and its Treatment by Peter C. Rowe, MD, Chronic Fatigue Clinic at the Johns Hopkins Children Center
POTS Diagnostics
Current diagnostic criteria and management of Postural Orthostatic Tachycardia Syndrome.
Fedorowski, A. (2018). Postural orthostatic tachycardia syndrome: Clinical presentation, aetiology and management. Journal of International Medicine, 285(4), 352-366.
POTS Diagnostics
A handy 1 page guide to POTS for Health Professionals
Author: Prof Lesley Kavi, Published 19/04/2020 potsuk.org
EXTRA RESOURCES...
CCI Support has been following research from around the world for over 4 decades. This link will take you to what we feel is some of the most reputable sites for information of Chronic Fatigue Syndrome and related disorders.
Medical Research
As an agency, we like to keep up to date with the research going on around the world. Here are some articles of interest.
Update on the DecodeME Study
The DecodeME team has just released the first results from the world’s largest ever genetic study of ME/CFS. Over 15,500 people with ME/CFS and more than 259,000 people without it took part. This makes it the biggest and most detailed look so far at whether our DNA...
A New Sleep Study Could Change What We Know About ME/CFS
For people with ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome), one of the most common and frustrating symptoms is unrefreshing sleep—sleep that doesn’t help them feel rested or better. Despite how important sleep is, researchers haven’t studied this part...
Transcutaneous Electrical Nerve Stimulation (TENS) as a potential option to bring relief from Fibromyalgia symptoms A recent American study by Zulbaran-Rojas et al (2024) found that Transcutaneous Electrical Nerve Stimulation (TENS) provided relief for...
Effect of Dietary Coenzyme Q10 Plus NADH Supplementation on Fatigue Perception and Health-Related Quality of Life in Individuals with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Prospective, Randomised, Double-Blind, Placebo-Controlled Trial...
Research: Cold Exposure and Cryotherapy in ME/CFS, Fibromyalgia, and Long COVID
This article explores the surprising potential of cold exposure therapies—including ice baths, cold showers, and whole-body cryotherapy (WBC)—as a supportive treatment for individuals with ME/CFS, fibromyalgia (FM), and long COVID. Though the idea of stepping into...
Inspiratory muscle training improves autonomic function
Inspiratory muscle training improves autonomic function in myalgic encephalomyelitis/chronic fatigue syndrome and post-acute sequelae of SARS-CoV-2: A pilot study – by Heather Edgell et al. (2025). Edgell, H., Pereira, T. J., Kerr, K., Bray, R., Tabassum, F., Sergio,...
Potential Benefits of Probiotics in Long COVID:
The paper "Long COVID and its Management" by Cheng Koc et al (2022) discusses multi-factorial suggestions for the management of Long COVID symptoms. One of the points discussed is the potential benefit of the use of probiotics. Here's a summary of the potential...
Inspiratory muscle training
Inspiratory muscle training improves autonomic function in myalgic encephalomyelitis/chronic fatigue syndrome and post-acute sequelae of SARS-CoV-2: A pilot study Edgell, H., Pereira, T. J., Kerr, K., Bray, R., Tabassum, F., Sergio, L., & Badhwar, S....
Development of an ME/CFS Online Screener
Research Article February 2025 Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is asevere and complex condition that significantly impacts daily life, leaving many individuals struggling with debilitating fatigue, post-exertional malaise (PEM),...
POTS is not FND
Postural orthostatic tachycardia syndrome and other common autonomic disorders are not functional neurologic disorders Full Opinion Article:...
Let’s talk
If you’d like to learn more about any of our services, or get involved, we’d love to hear from you.