Looking well but feeling extremely unwell?
Do you suffer from…
Persistent fatigue?
Muscle or joint pain?
Impaired memory & concentration?
Disturbed sleep patterns?
Digestive issues?
Our support service may be able to help
As a community health agency that supports people with Chronic Fatigue Syndrome, Fibromyalgia and other related illnesses. Complex Chronic Illness Support has a vision to “Empower People Towards Wellness” and our purpose is to improve the quality of life of people who suffer from a complex chronic illness, as well as that of their loved ones.
Illnesses We Support
Myalgic Encephalomyelitis (ME) / Chronic Fatigue Syndrome
Myalgic Encephalomyelitis, also known as Chronic Fatigue Syndrome (together referred to as ME/CFS), is a debilitating, long-term, multi-system illness. It can affect the immune, neurological, endocrine, and autonomic systems, leading to a wide range of confusing and disabling symptoms. It has been described as an abnormal immune system response to any number of infectious or environmental triggers, causing a long-term illness that can result in significant disability.
Known triggers are viral infection, or a myriad of triggers, including but not limited to adverse/allergic reactions to anaesthesia/vaccination, chemical toxicity, hormonal fluctuations (childbirth, menopause), physical/emotional trauma, and/or genetic predisposition. There is also emerging research to show genetic links.
Approximately 80% of cases are preceded by a viral infection, such as:
- Common cold
- Influenza
- Pneumonia
- Epstein-Barr virus/Glandular fever
- Herpes virus
- COVID-19
While many people recover from viral illness within a few weeks, those with ME/CFS do not return to full health and instead develop persistent, life-altering symptoms lasting at least six months prior to diagnosis for adults, and three months for children.
In the case of COVID-19, symptoms lasting beyond twelve weeks may be diagnosed as Long-COVID, and if they persist beyond two years, they may be considered Long-COVID–induced ME/CFS.
People who have compromised/weakened immunity or have pre-existing conditions may be more prone to ME/CFS. At present, there are few treatment options available for ME/CFS.
- Onset: Can be triggered by a viral infection, but it can also have a gradual onset without a clear viral trigger.
- Symptoms: Prolonged and severe fatigue, often accompanied by cognitive dysfunction (brain fog), unrefreshing sleep, and pain. The symptoms are not solely explained by ongoing viral activity or other medical conditions.
- Duration: ME/CFS is characterised by persistent symptoms that last for at least six months. The severity of symptoms can fluctuate, but the condition is chronic, lasting for years.
It's important to note that while post-viral fatigue can resolve on its own as the body recovers from the initial infection, ME/CFS is considered a chronic condition with a more persistent and often disabling course. The defining diagnostic characteristic of ME/CFS is post-exertional malaise (PEM) – a worsening of symptoms after even small amounts of physical, mental, or emotional effort, often delayed by 24–72 hours.
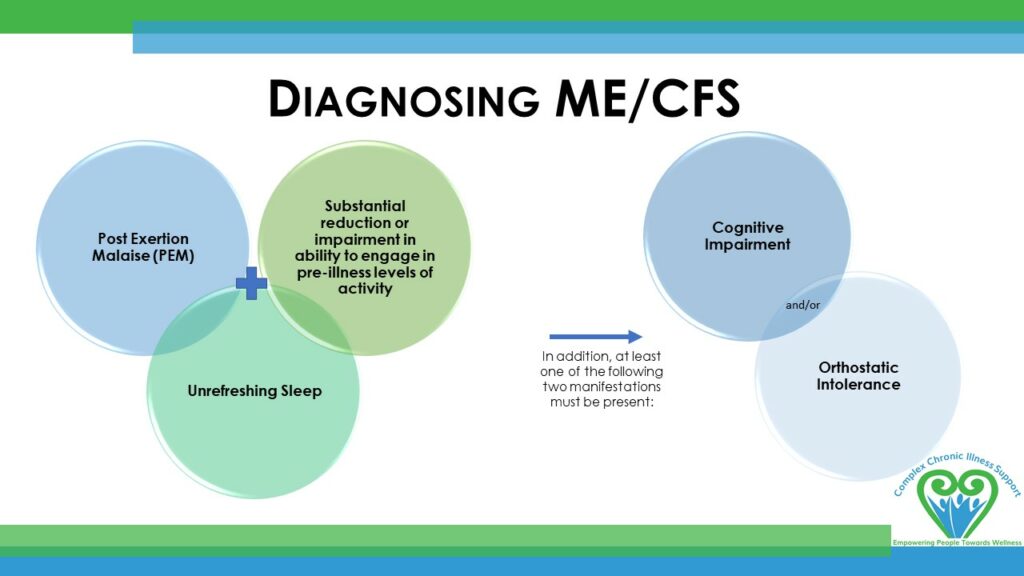
Main symptoms include:
- PEM
- Unrefreshing sleep
- Unrelenting fatigue that cannot be explained by other conditions
- and then 1 of: Orthostatic intolerance or cognitive impairment – impaired memory and concentration.
- Muscle and/or joint pains
- Sleep disturbance
- Digestive problems
- Sensitivities to light and sound
- Headaches/migraines
- Sore throat and/or enlarged lymph nodes
- Dysregulated temperature control – fever/chills
- POTS
- Orthostatic intolerance – erratic heart rate, feeling faint or dizzy upon standing
- Anxiety and/or irritability
- Up to 100-200 symptoms based on body system involvement
Currently, there is no single diagnostic test; however, there are set exclusionary accepted international criteria for diagnosis. Currently, there is no known cure. Management focuses on symptom relief, pacing, and supportive care. ME/CFS can last for years and ranges in severity from mild (limiting daily activities) to very severe (bed-bound and dependent on others for care).
Treatment
Treatment for ME/CFS is about managing symptoms and pain.
The key to symptom management is pacing.
If PEM (post-exertional malaise) is experienced, you must avoid exercise and activities that cause fatigue or increased symptoms and conserve your energy.
Long COVID
Long-COVID refers to a condition where symptoms persist or develop after the initial COVID-19 (SARS-CoV-2) infection, lasting beyond the expected recovery period. While most people recover from COVID-19 within a few weeks, some continue to experience ongoing and often disabling symptoms. This is sometimes called Post-COVID-19 Syndrome or “Long-COVID.”
The World Health Organization defines Long-COVID as symptoms that continue twelve weeks or more after infection and cannot be explained by another diagnosis.
Symptoms may include:
- Severe fatigue and exhaustion
- Post-exertional malaise (worsening of symptoms after activity)
- Cognitive difficulties (“brain fog”)
- Shortness of breath, chest pain, or heart palpitations
- Sleep problems
- Muscle and joint pain
- Autonomic issues such as dizziness or rapid heart rate (POTS/orthostatic intolerance)
- Sensory issues such as loss of taste or smell
- There are up to 200 symptoms based on body system involvement.
- A diagnosis of Long-COVID does not require the same degree of functional impairment (such as a 50% or greater reduction in physical and mental activity) that is required for a diagnosis of ME/CFS.
Prevention of Long-COVID
Prevention: After COVID-19, many people are eager to regain their health and return to normal life as quickly as possible. However, evidence shows that pushing too hard—whether physically or mentally—during the recovery phase can worsen symptoms, prolong recovery, or even lead to a diagnosis of ME/CFS. It is therefore vital to pace yourself and take exceptional care during this time. Some individuals may be genetically more vulnerable to post-viral illness, and those already living with ME/CFS are at particular risk of relapse if they over-exert. These insights highlight the importance of rest, gradual recovery, and self-compassion for anyone recovering from COVID-19.
Types of Long COVID
- Long-COVID (mixed symptoms): The largest group, experiencing a combination of symptoms directly related to COVID-19 (such as respiratory or cardiac problems) alongside symptoms that overlap with ME/CFS.
- Post-COVID ME/CFS: A smaller group whose illness is indistinguishable from ME/CFS, with no ongoing COVID-specific symptoms. This group develops ME/CFS following COVID-19.
- Long-COVID with COVID-only symptoms: A smaller group whose symptoms are only related to COVID-19 complications (e.g., lung scarring, clotting issues) and do not include ME/CFS features. As an ME/CFS support service, we do not support this group.
Occasionally, individuals may develop a chronic post-immune condition following vaccination, with symptoms overlapping those of ME/CFS. In such cases, this may be described as vaccine-triggered ME/CFS, rather than Long-COVID.
Progression
- Symptoms that last longer than twelve weeks after COVID-19 onset may be diagnosed as Long-COVID.
- If symptoms remain beyond eighteen months, particularly when ME/CFS features are dominant, a diagnosis of Post-COVID ME/CFS may be appropriate.
Treatment
Treatment for Long-COVID is similar to that of ME/CFS. It is about managing symptoms and pain.
The key to symptom management is pacing.
If PEM (post-exertional malaise) is experienced, you must avoid exercise and activities that cause fatigue or increased symptoms and conserve your energy.
The ME Association in the UK has developed a document to discuss whether ME and Long-COVID are the same condition: https://meassociation.org.uk/literature/items/long-covid-and-me-cfs-are-they-the-same-condition/
Fibromyalgia
Fibromyalgia is a chronic condition characterised by widespread musculoskeletal pain, fatigue, and heightened sensitivity to touch, pressure, or other stimuli. It affects the nervous system, altering the way the brain processes pain signals, and can lead to a variety of physical and cognitive symptoms.
The cause of Fibromyalgia is thought to involve a combination of genetic, neurological, and environmental factors, including previous infections, physical trauma, or emotional stress. It often occurs alongside other chronic conditions, including ME/CFS.
People with Fibromyalgia generally experience pain in specific points around the body. These points are no longer used to gauge for diagnosis; however, it is a helpful way of explaining where people are likely to feel pain.
(See https://www.healthline.com/health/fibromyalgia/fibromyalgia-tender-points for more information.)
The points around the body are:
- Back of the head
- Area between the shoulders
- Front of the neck
- Top of the chest
- Outside of the elbows
- Top and sides of the hips
- Insides of the knees
Typical features include:
- Widespread, persistent pain in muscles, ligaments, and joints
- Fatigue and low energy
- Sleep disturbances and unrefreshing sleep
- Cognitive difficulties, often called “fibro fog” (memory and concentration issues)
- Headaches or migraines
- Sensitivity to light, sound, temperature, or touch
- Irritable bowel symptoms or other digestive issues
- Mood changes, including anxiety or depression
Onset and course:
- Fibromyalgia can develop gradually over time or after a triggering event such as infection, injury, or significant stress.
- Symptoms fluctuate in severity, and flare-ups may be triggered by stress, physical activity, or environmental factors.
- Fibromyalgia is a long-term condition, and while there is currently no cure, management focuses on symptom relief, pacing, lifestyle adjustments, and supportive care.
Post-Viral Fatigue / Syndrome
Post-Viral Fatigue (sometimes called Post-Viral Fatigue Syndrome, PVFS) is a condition where fatigue and other symptoms continue well beyond the expected recovery time after a viral infection. In most straight-forward viral illnesses, recovery takes 2–4 weeks, with symptoms disappearing by six weeks. However, a small percentage of PVF/S patients may take several months to recover.
Typical features include:
- Persistent fatigue and lack of energy
- Reduced tolerance to activity (physical or mental)
- Poor concentration or “brain fog”
- Unrefreshing sleep
- Muscle aches or generalised pain
- Slower recovery from exertion
For many, PVF/S improves gradually over time as the body heals. If symptoms persist for at least six months in adults, or three months in children, and there is no significant improvement, the condition may be diagnosed as Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS).
Dysautonomia
Dysautonomia is a term for a group of diseases that include Postural Orthostatic Tachycardia Syndrome (POTS), Neurally Mediated Hypertension (“NMH”) and Orthostatic Intolerance (OI).
In these conditions, the autonomic nervous system (“ANS”) is dysregulated, which can lead to blood pressure problems, heart problems, trouble with breathing and swallowing, and erectile dysfunction in men.
Postural Orthostatic Tachycardia Syndrome (POTS)
Main symptoms include:
- Fatigue
- Headaches
- Light-headedness and dizziness
- An extreme increase in heart rate upon moving from a supine position to sitting position or standing position (extreme defined as over 100bpm). Diagnostic criteria involves if it rises by 30bpm in adults or 40bpm in youth, within 10 mins of standing. For most individuals living with POTS, this means experiencing an increase in heart rate above 100 to 200 compared to the expected heart rate of 60.
- Exercise intolerance
- Nausea
- Diminished concentration and forgetfulness
- Tremulousness (shaking)
- Coldness or pain in the extremities
- Excessive sweating
- Chest pain and shortness of breath.
- Sleep difficulties
- Anxiety (as an autonomic dysfunction)
Neurally Mediated Hypertension (“NMH”)
Abnormal reflex lowering of blood pressure during upright posture (low blood pressure created via the nervous system).
- Low blood pressure from faulty brain signals / ‘miscommunication’ between the heart and brain.
- Causes blood pressure to drop when a person has been standing for long periods, which is the opposite of what is needed, i.e. for the heart to beat faster to pump blood back up to the brain. Many people will not be able to “stand still” and they will walk to pump their legs in an attempt to push blood back up to the heart unconsciously.
- Leads to dizziness, nausea, and fainting.
Dr. Vallings refers to this as “3rd aisle of the supermarket;” after getting from the car to the supermarket and around a few aisles, fainting and falling becomes a possibility as there is a sudden feeling of the plug being pulled, marked by nausea, dizziness, fatigue, and brain fog.
Orthostatic Intolerance (“OI”)
POTS and NMH both have Orthostatic Intolerance as their primary symptom.
Orthostatic Intolerance is an umbrella term for the development of symptoms when in an upright posture.
OI can be caused by standing in an upright position for long periods of time, after being in a warm environment, immediately after exercise, after an emotionally stressful event, after eating (blood flow moved to digest food), or if salt and fluid intake is inadequate. These symptoms subside when returning to a horizontal position.
Symptoms of OI include:
- Light-headedness
- Altered vision
- Headache
- Heart palpations
- Exercise Intolerance
- Fatigue
- Neurocognitive deficits
- Anxiety
- Nausea
- Abdominal discomfort
- Tremulousness
- Sweating
- Weakness
- Syncope (fainting)
Related Condition
Mast Cell Activation Syndrome (MCAS)
Please note: we do not support MCAS as a stand alone condition. This requires GP support. We do however support MCAS when it is a part of the conditions above.
MCAS is a condition where mast cells misfire, causing systemic symptoms. It appears to overlap with ME/CFS and Fibromyalgia in a substantial subset of patients, potentially contributing to fatigue, brain fog, pain, dysautonomia, and hypersensitivities.
- Mast cells are immune cells that play a role in allergy and inflammation.
- In Mast Cell Activation Syndrome (MCAS), mast cells release chemical mediators (such as histamine, prostaglandins, and cytokines) inappropriately or excessively.
- Mast cells are also involved in tissue repair (which is why those with ME/CFS have too many, due to sleep dysregulation as sleep is when tissue repair occurs). They are also involved in blood flow regulation, which explains the overlap in ME/CFS as well as dysautonomia. In addition, mast cells are involved in the immune response to pathogens, therefore explaining why MCAS is a common co-morbid condition with ME/CFS because the dysfunctional immune system either attacks everything in hyperdrive or allows pathogens in.
- This leads to symptoms across multiple body systems, such as:
- Skin: flushing, itching, hives
- GI tract: nausea, abdominal pain, diarrhoea
- Cardiovascular: dizziness, low blood pressure, increased heart rate
- Neurological: brain fog, headaches
- Respiratory: shortness of breath, throat tightness
Unlike classic allergies, MCAS reactions often don’t show up on standard allergy tests, although there is a common misconception that it is an allergy response due to the release of histamine. Histamine is also part of inflammatory response, sleep-wake cycle, and gastric acid secretion, which is why those with severe chronic illness often experience serious gastrointestinal issues.
MCAS and ME/CFS
- There’s growing evidence that a subset of people with ME/CFS also have mast cell dysregulation.
- Proposed connections:
- Neuroinflammation: Mast cells can activate microglia in the brain, contributing to fatigue, pain, and cognitive issues.
- Autonomic nervous system (dysautonomia): Histamine and mast cell mediators may worsen POTS (Postural Orthostatic Tachycardia Syndrome), which is common in ME/CFS.
- Post-viral triggers: Infections that trigger ME/CFS may also disturb mast cell regulation.
- Overlap in symptoms: Fatigue, brain fog, gastrointestinal upset, and sensitivity to stimuli are shared features.
Some researchers think mast cell dysregulation may be one of the drivers in a subset of ME/CFS patients.
MCAS and Fibromyalgia
- In Fibromyalgia, mast cells have been found near pain nerve fibres.
- Their release of histamine and cytokines may amplify pain signalling and sensory hypersensitivity.
- This could help explain widespread pain, skin sensitivity, and poor sleep in some patients with Fibromyalgia.
Exact prevalence is unclear, but studies and clinical observations suggest a significant overlap between:
- ME/CFS and MCAS
- Fibromyalgia and MCAS
- ME/CFS, Fibro, MCAS, and POTS (sometimes called “the quartet”).
“Histamine Intolerance” is very common in the very severe cases, with potential symptom management on low histamine diets and medication.
Management
People with both ME/CFS or Fibro and MCAS may find some improvement with:
- H1 antihistamines (cetirizine, loratadine)
- H2 antihistamines (famotidine, ranitidine [no longer widely available])
- Mast cell stabilisers (cromolyn sodium, ketotifen, quercetin)
- Low-histamine diet or avoiding known triggers (heat, stress, certain foods, chemicals)
Treatment is usually trial-and-error and guided by a knowledgeable doctor. As this requires Medical Intervention, supporting MCAS as a stand-alone illness falls outside the scope of our capacity to provide effective supports as CCI Support predominantly offers social support services. While we cannot support this condition as a stand-alone illness, we will however support people with the condition, when it is co-occurring with one or more of the illnesses we do support.
An Existence Project
A paper stop-motion animation about what it’s like to live with mild or moderate ME/CFS. Inga made this short film so people would have something they could show their friends and family to help them communicate the complex aspects of living with this chronic illness. Created by: Inga Topolnicki and added to our website with direct permission.
What services we provide:

To ask for help, please complete the Referral form
CCI Support is now a national service. We can work with people throughout New Zealand. Tauranga, Hamilton and Wellington have local Facilitators, all other areas are currently supported online and via phone at this stage.
We also offer support for family and friends of people living with the conditions that we support. The person does not have to be a current CCIS member.
Frequently Asked Questions
Who is CCI Support?
CCI Support (Complex Chronic Illness Support) is an Incorporated Society*, not for profit in New Zealand.
We have qualified staff in Tauranga, Whakatane, Rotorua, Nelson, Waikato, and Wellington, and also provide remote and virtual support to all other parts of New Zealand.
Our administrative office is based in Tauranga. Consisting of a facilitator support administrator, a funding team, and a CEO.
We have six members, placed throughout the North Island, that bring together business acumen and support to maintain the forward-thinking services that this agency has provided for over 41 years.
Whilst we are the largest one-on-one support service for people with ME/CFS in New Zealand, the reality is that we are made up of many smaller regional groups, providing personalised support and care for people with ME/CFS and FM. This is achieved through a fabulous bunch of volunteers placed throughout the country to facilitate social groups and provide support for the Facilitators, as well as manage our social media.
As an incorporated society, we are member-focused. Members vote on constitutional changes, members pay an annual fee, and have the ability to bring communication to the CEO and Board, on how CCI Support is run. An AGM is held in September annually.
To be a member of CCI Support there is a small annual fee of $45. This fee helps our Funders understand how much our members respect and support the work we do. This in turn often means that they are more likely to be generous with their funding toward us. Leading us to develop and provide the services we do. This fee can be paid off for as little as $1 per week. Members can also get support from the Ministry of Social Development via the Disability Allowance or Temporary Additional Support, if their GP signs it off.
- An incorporated society is a membership-based organisation that has registered under the Incorporated Societies Act 1908
What do we do?
We provide qualified one on one facilitator and group support to people with Myalgic Encephalomyelitis (Chronic Fatigue Syndrome/CFS), Fibromyalgia (FM), some Dysautonomia’s (POTS and Orthostatic Intolerance), and Long COVID.
We are well aware that these conditions do not stand alone, that they often come with co-morbidities. We are NOT a medical agency; we are a social support agency. This means that we can work with the entire family and be holistic in our care. We support the medical care provided by health professionals and allied health professionals. We can also provide names of specialists you can access.
We walk alongside our members on their journey towards wellness (whatever wellness may look like for them). We provide holistic and completely non-judgemental support.
We teach symptom management and provide the resources to give members a personalised toolkit to manage their condition, within their capacity/capabilities. With our support, people with complex chronic illnesses can, in time, develop an increased ability to participate in family, social and community life, and lead a life that is fulfilling and meaningful for them.
We also provide low-level advocacy for people needing support with Health Professionals, MSD, and workplaces, as required.
CCIS works within the Te Whare Tapa Wha framework, this model focuses on the four cornerstones of health. Should one of the four dimensions become damaged or missing, the person’s sense of well-being is unbalanced, this is not a healthy state. We work holistically to support each member and their loved ones, understanding that each of the four cornerstones are important to their well-being.
- Taha tinana (Physical health)
- Taha wairua (Spiritual health)
- Taha whanau (Family health)
- Taha hinengaro (Mental Health)
We can work with family/Whanau and supportive friends of people living with chronic illness. We explain to loved ones, how this illness affects people and how they can best be of support. We provide them with a deeper understanding of what this person is going through.
Please be aware our resources are stretched and are provided by Grants and Donations. But in all aspects, we are good stewards with the money that does come in. ALL money is accounted for and is used to provide support directly to members. We do not hold onto any profit.
What Services do we provide?

Health and Wellness Facilitators
We have qualified Health and Wellness Facilitators based in the Bay of Plenty, Wellington and Waikato and virtually throughout NZ who work with members and the community to provide support, mentoring, advice, counselling, and advocacy. This essential role is undertaken through home visits, and phone and online contact, in addition to guidance and support through regular support group meetings, education sessions, access to counselling service and the CCI Support library and newsletters.
Our Staff have a range of qualifications including
- Comprehensive Nurse (Psych and General)
- Counsellor / Diploma in Health & Human Behaviour
- Bachelor of Community Health / Diploma of Rehabilitation
- Bachelor of Science / Teachers Diploma / Mindfulness Coach
- Masters in Health Psychology / Bachelor of Science with Clinical & Health
Support Group Meetings
The support group meetings offer the opportunity for members to have a group catch-up with our Health and Wellness Facilitators, and to share ideas and support with one another. The objective of the group meetings is to give members access to tools and resources to enable them to develop their own solutions to issues, and manage their own illness, developed from conversations in a confidential and safe space.
Social Groups
The CCI Support social groups are locally placed around NZ and also available online. Once you are a member, you will be given all the details for the groups available to you.
Online Support and Resources
We have a Members Only section on the website, it gives links to:
- Meeting information (Educational and Social)
- Resources for managing symptoms
- Forums to connect with other members and ask questions
- Newsletters and information about what is going on in CCIS
- Regional updates for the Facilitators – so you know what’s happening in your area
Towards Wellness Programme
The CCI Support Towards Wellness Programme offers the best of research-based knowledge into an easy-to-understand package to help people living with complex chronic illness begin to find their next steps towards wellness. Participants learn foundation principles to assist them in navigating their journey, and in creating an individual road map to support increasing health and wellness.
The programme is the first of its kind in New Zealand, winning the Highly Commended Innovative Provider Award at Adult Learner’s Week in 2016, and is endorsed by New Zealand’s leading authority on CFS /ME, Doctor Ros Vallings.
The course structure comprises two hours fortnightly (in total 10 workshops) based at the premises of CCI Support, or, more recently online with the impact of COVID-19, with a follow-on 5 workshops to reinforce key learnings. Guest speakers are also invited, and include a nutritional coach, physiotherapist, and general practitioner. Workshop topics include Understanding the Conditions, Systems and Stages, Pacing – Balancing Activity and Rest, Stress Management, Sleep, Nutrition, Pain Management – A GP’s Perspective, and Building Your Support Network.
Towards Wellness Hub
The Towards Wellness Hub is an online knowledge base of content, resources, and services, available 24/7 for those in the community with Myalgic Encephalomyelitis / Chronic Fatigue Syndrome, Fibromyalgia, Dysautonomia, and Long COVID, their whānau, and their communities, throughout New Zealand. It’s also a resource for health professionals and other organisations and individuals who wish to learn more about complex chronic illness. The Towards Wellness Hub is a new way of delivering the resources and services of CCI Support to clients and interested parties, which they can access as needed, from their own home and environs. As with many health issues and disabilities, the hardest time to cope is when people are alone. With access to the hub, clients can feel accepted and safe, with access to a familiar support system at their most vulnerable times.
There is an extra cost of $200 for this course.
Community Workshops
Complex chronic illnesses affect not only the individual, but also those people around them. Compounded by illnesses where symptoms and their effects fluctuate, and which are hard to manage, difficult to understand and often misunderstood, can prove to be challenging for whanau, friends, carers, and the wider community. CCI Support provides workshops to assist in educating those surrounding an individual so they can understand and support their loved ones.
Advocacy and Awareness
At CCI Support we are continually striving to raise awareness of all complex chronic illnesses. Increasing awareness is a key goal, ultimately enabling us to support more people, increase our membership and develop our services further. Recently this included meeting with local MPs to discuss party policies and support with regard to complex chronic illness.
We provide low level advocacy, by providing supportive documentation and support for meetings with health practitioners, WINZ, family members and members workplaces, where appropriate.
Online Support – Facebook Community
CCI Support has an active online community, comprising two Facebook pages – a public page to raise awareness, and a closed private members page to provide connections and reduce isolation, providing a way to keep in contact and give group support to each other.
Newsletters
CCI Support creates and distributes a comprehensive newsletter to our members, including up-to-date research, information, strategies, techniques, wellness stories, plus links to events and meetings. This is a key tool to keep members involved with our organization and other members.
Library
We offer a comprehensive library service to our members, with access to specialised books and information to help them through their journey to wellness. We hope to develop this further in the coming year and make it more easily accessible to more members.
Group Seminars
We provide events, specialised speakers, doctors, nutritionists, mindfulness coaches, physiotherapists and other experts in this area.
How do we achieve this?
A person comes to CCIS, either via a self-referral, GP referral or a family member reaching out asking for help. They are then assessed to see if their condition fits within our illness parameters. We then ask for the person to become a member, so that they are able to get the support we provide.
We then provide a telephone or telehealth appointment that is 30-45 mins long, this is where we hear their story, assess their needs and then provide some support, advocacy and tools to help them manage their symptoms.
Our Facilitators encourage attendance to the online support group. These are held and are themed educational sessions provided via zoom (easy click link access). Research suggests the importance of social connection is beneficial to a person’s wellness journey.
As a charity, our funds are EXTREMELY limited and group education is a way we can be good stewards of our resources, as well as connecting our members with other people going through a similar journey to themselves.
4-6 weeks after a support assessment (or at a time agreed upon) the facilitator will contact the member back, to see how they are going, reassess their personal goals and provide more tools, strategies and a plan moving forward.
What else do we ask of you?
We highly recommend that our members attend a social group, these are available in person in some regions, otherwise, we have a few online ones (men’s, women’s, mums, young people etc). Often one of the first things to go when someone is unwell is their social support system. As a human, personal interaction is incredibly important, to have someone in their corner that completely understands can be very encouraging.
There are mindfulness/meditation groups that meets virtually, as well as breathing and restorative movement short videos to help you.
We have a private group on Facebook where members can reach out to others in a similar situation for advice, support, and just a connection with someone else who “gets it.” We understand that our members can have maladjusted circadian rhythms, and although our facilitators are only available during office hours, within the private Facebook group there are other members to talk to. This group is moderated by volunteers. We recommend 1737 is used for counselling needs.
We have counsellors available at times to provide free counselling. We are in the process of trying to raise the funds to get a counsellor on staff.
The Towards Wellness Programme is currently being held online. It covers many topics that are incredibly important or relevant to those with ME/CFS and FM. This can be done in a person’s own time, and at their own pace – in bite-size pieces that support your energy envelope requirements. This also includes a monthly zoom catch-up to ask facilitators any questions. This programme is highly recommended and was endorsed by Dr Ros Vallings. In 2016 the programme won a local Adult Learning Innovative Provider Award.
Wellness does not mean perfectly healthy. It means your health is at a level where you can manage your life, develop an increased ability to participate in family, social and community life, and lead a life that is fulfilling and meaningful.
We find that members who (within their limitations) join in with one-on-one support, group meetings and social groups progress on their journey towards wellness more effectively than those who try to go it alone.
Suggesting loved ones also join in on a member’s wellness journey, helps them to support our members in their own environment. This then makes long-term progress towards the life that our members find meaning in.
Do you know of any GP’s who understand ME/CFS/FM/POTS, in my area?
At CCI Support, we prioritise the wellbeing and privacy of both our members and health professionals. We do not provide recommendations for any GP or other health professional, nor do we advise our members against pursuing care with any GP or other health professional. Any information shared serves to connect our members to possible resources to explore in their area. Please contact your facilitator for resources available in your area that have been reported to be helpful based on feedback from our members.
Where are you in New Zealand?
We have Facilitators in
- Tauranga / Western Bay of Plenty
- Whakatane / Eastern Bay of Plenty
- Waikato
- Wellington
- We also provide remote services to all of New Zealand, via way of phone calls, telehealth appointments and online support and social groups.
Do you provide advocacy services?
We provide low level advocacy services. Letters to take to employers, schools, Health Professionals, MSD etc. If you have a local facilitator in your area, we may be able to attend some appointments with you.
Do you support other conditions?
Unfortunately, we do not have the expertise to support chronic pain conditions, rather we support illnesses which may have a pain component. If you have a condition that sits outside our scope of practice, please find below links for helpful information and support
Arthritis https://www.arthritis.org.nz/
https://www.healthnavigator.org.nz/health-a-z/o/osteoarthritis/
Chronic pain
https://www.healthnavigator.org.nz/health-a-z/c/chronic-pain/
There are many chronic pain groups on Facebook to choose from: FACEBOOK SEARCH
You may also be eligible for a referral with the Tauranga pain clinic which can be accessed through your GP
Do you offer any support to non-members?
We are a member based charity service. All of our services are available to members only. We ask for a nominal $45 pa joining fee (which covers the April to March financial year). This gives you access to the services provided. Some courses may have extra charges.
I am in a crisis and need support NOW
CCISupport is not an acute service, so in a crisis please contact your GP.
Where to find other help and Support
- Need to talk? 1737 or text 1737 for support from a trained counsellor
- The Depression Helpline: 0800 111 757 or free text 4202
- Healthline: 0800 611 116
- Lifeline: 0800 543 354
- Samaritans: 0800 726 666
- Youthline: 0800 376 633 or free text 234 (8am-12am), or email [email protected]
- The Lowdown: thelowdown.co.nzor free text 5626
- Kidsline (ages 5–18 years): 0800 543 754
- OUTline NZ: 0800 688 5463 for confidential telephone support for the LGBTQI+ family, as well as their friends and families
- Alcohol Drug Helpline: 0800 787 797 or free text 8681
- Gambling Helpline: 0800 654 655 or free text 8006
- What’s Up? whatsup.co.nz (for 5–18 year olds). Phone counselling is available Monday to Friday, 1pm–10pm and weekends, 3pm–10pm. Online chat is available 7pm–10pm daily.
- Womens Refuge: https://womensrefuge.org.nz/ 0800 733 843
- Shine: Domestic Abuse Services: https://www.2shine.org.nz free call: 0508 744 633 (9am and 11pm)
- Hey Bro: https://www.hewakatapu.org.nz supporting men to be free from violence 0800 HeyBro (439 276)
- Family violence information line Areyouok.org.nz to find out about local services or how to help someone else: 0800 456 450
- Need to talk? Free call or text: 1737 for mental health support from a trained counsellor
- Youthline: Youthline.co.nz: 0800 376 633, free text: 234, email: [email protected]
- Shakti – for migrant and refugee women – 0800 742 584 – 24 hours
- Elder Abuse Helpline 0800 32 668 65 – 24 hours
In an emergency
If it is an emergency and you feel that you or someone else is at risk:
Call 111 or Go to your nearest hospital emergency department (ED) or Call your local DHB Mental Health Crisis Team (CATT) 0800 611 116 and stay until help arrives. If someone is unconscious, call an ambulance (111).
How can I contact my Facilitator?
Via email, phone or text. If calling outside of work hours, please leave a message and your Facilitator will be in touch at their earliest convenience.
Office hours are Tuesday to Friday 9am – 2.30pm
0800 224 787 or text 022 658 0251
Our Blog
Our Blog has some wonderful stories and encouraging words from other members. It’s well worth checking out.
“Before I Got Sick” – A Poem by Frances Hellendoorn
Before I got sick, I did not realise we had birds in our garden. I did not know that the myna has a hilarious bob in his song. That my ‘happy place’ bird from my childhood is a barbary dove and likes to ‘hang out’ on the power lines and gutter opposite our house in...
“Invisible Dragons” – A Poem by Frances Hellendoorn
Everyday I fight Invisible Dragons. My disability fences me in. But to all but a few the fences are invisible. I sat on the store furniture because I could not walk all the way around the store. No customer courtesy chair was provided. I am not old, although I...
Tapping – Shifting the Urge to Rush into a Calm, Healing State
By Annabelle Tapping or EFT (Emotional Freedom Technique) is a self-help technique designed to reduce stress/anxiety. It involves gently tapping specific points on the face and body while focusing on the emotions or stress you wish to let go of. EFT may help in...
Let’s talk
If you’d like to learn more about any of our services, or get involved, we’d love to hear from you.